Anterior Approach Hip Replacement
A minimally-invasive muscle-sparing hip replacement approach for faster recovery.
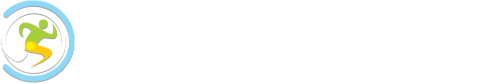
Anterior Minimally Invasive Surgery (AMIS)
In contrast to traditional hip replacement techniques where the patient lies on their side and the incision is made through muscles on the side or back of the hip, the Direct Anterior total hip replacement uses a front (anterior) approach with the patient positioned on their back (supine).
The surgery is conducted between the front muscles of the hip, eliminating the need to detach muscles on the side or back off the hip.
The gluteal muscles at the side of the hip and the short rotator muscles at the back of the hip play a crucial role in balance and walking, and avoiding surgical disruption of these muscles can lead to a faster recovery post-operation.
Dr Frederic Laude (under whom Mr Freedman trained in Paris) revolutionised hip surgery by developing an innovative new operating table and specialised instruments, which allows surgery to be conducted between muscles via an anterior approach
Additionally, with the patient lying on their back (supine), real-time x-rays can be taken during the procedure to confirm the correct placement of the implant and to assist leg length measurement, aiding the surgeon in achieving the best possible outcome.
A range of benefits
Key advantages of the supine position technique in hip replacement surgery include:
- Smaller Incision: The incision is typically only 6-8cm, much smaller than the >15cm typical for other approaches.
- Preserved Posterior Structures: The posterior capsule at the back of the hip is not opened during surgery, keeping the posterior structures intact and greatly reducing the risk of posterior dislocation (near zero).
- Quick Rehabilitation: The stability of the hip post-surgery allows patients to rehabilitate very quickly, instilling confidence in their ability to recover.
- No Post-Operative Restrictions: Patients undergoing this technique generally require no post-operative restrictions and are allowed to sit in regular chairs, cross their legs, and sleep on their sides.
- Reduced Discomfort and Medication Needs: With no major muscle releases or incisions required, post-operative discomfort and the need for pain medication are often reduced.
- Avoiding Side Effects: Minimising the use of strong analgesics helps avoid side effects like nausea, drowsiness, and constipation.
- Accurate Surgery with X-ray Assistance: Performing surgery with the patient lying on their back allows the use of X-rays during the procedure to check the position of the implants and leg length, facilitating accuracy.

Case Examples
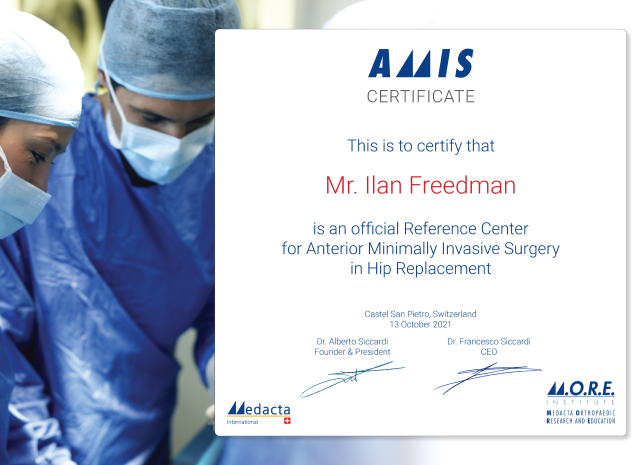
Mr Freedman’s training & experience

An Internationally-trained and renowned Orthopaedic surgeon, Mr Freeman brings over a decade of experience to providing a meticulous standard of care.
The success of technically complicated surgery depends on several elements, but one important factor is having a highly-trained and experienced surgeon.
Mr Freedman completed a fellowship in the UK to train in hip arthroscopy with Professor Damian Griffin, a world-renowned expert in hip arthroscopy and hip preservation surgery.
While on fellowship in the UK, Mr Freedman’s supervisor, Professor Griffin, received an invitation to observe a new hip replacement technique in Paris with Dr. Frederic Laude, a world expert in Direct Anterior hip surgery. As fate would have it, other commitments prevented Prof. Griffin from attending, so he sent Mr Freedman in his place, and he was amazed by the innovative procedure, the minimal incision, and the quick recovery of patients. Mr Freedman later returned to Paris to complete a fellowship under Dr Frederic Laude.
Upon returning to Australia, Mr Freedman, successfully implemented anterior approach hip replacements in his practice, leading to rapid growth in his case numbers and the eventual standardisation of this technique, even for complex surgeries.
-
Internationally Trained and Recognised
Mr Freedman has trained under some of the best hip surgeons in Europe.
-
Cutting-Edge Techniques
Mr Freedman employs advanced technology and techniques to ensure the best possible outcomes for his patients.
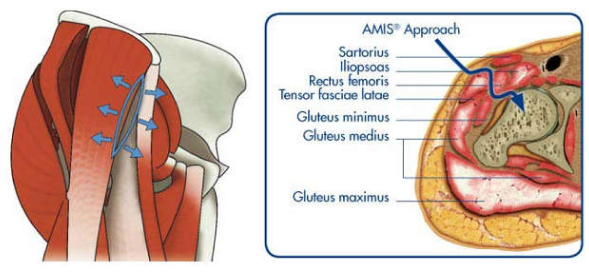
Making advanced techniques possible
Mr Freedman strives to stay up to date with new developments in technique and technology to provide the best care for his patients. He is committed to continuous learning and regularly updates his skills and knowledge in the field.
By using the latest techniques and implants, he ensures that his patients benefit from the most advanced and effective treatments available. This dedication to excellence allows him to achieve the best possible outcomes and maintain a high standard of care in his practice.
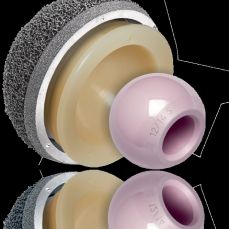
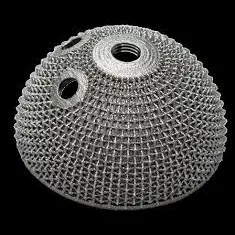
Hip Replacement Implants



Minimally invasive techniques for better recovery
Experience an easier recovery with our enhanced recovery pathway, designed to improve patient outcomes and speed up recovery following surgery. This approach reduces the need for pain medication and eliminates post-operative restrictions such as crutches, allowing you to be back on your feet sooner with a reduced risk of dislocation. Our pathway focuses on optimising every aspect of your journey, promoting you as an active participant in your recovery and rehabilitation to accelerate post-operative recovery and minimise complications.

Frequently asked questions
The best type of hip replacement for you depends on factors like your age, activity level, overall health, and specific hip condition, typically determined in consultation with your orthopaedic surgeon.
Mr Freedman utilises various enhanced recovery mechanisms so that you will be dressed in your normal clothes (and not a hospital gown) and up and walking the same day as your surgery. Patients are often safe for discharge Day 1 after surgery. However, there are some benefits of being in hospital a bit longer such as access to inpatient physiotherapy services and also being away from home responsibilities allows you to focus on your rehab and recovery. Therefore, Mr Freedman will often advise you not to rush home too quickly but rather to spend 2-3 nights in hospital so that you are confident and comfortable at discharge.
Mr Freedman uses a variety of implants, depending on individual patient anatomy, age and other considerations. The prostheses used most frequently are designed and manufactured in Switzerland. Mr Freedmam often favours ceramic bearing surfaces. These ceramic implants are manufactured in Germany. Just as the Swiss and Germans engineer and manufacture great watches and fantastic cars, they also make excellent hip and knee prostheses.
Mr Freedman completed University (Medical School) at the University of Melbourne and then Surgery and Orthopaedic Surgery training in Victoria, through the highly regarded Australian Orthopaedic Associations’s Victorian Training Program. After completing his orthopaedic training, Mr Freedman undertook two international orthopaedic fellowships. The first of these were with Professor Damian Griffin in the UK (University Hospital Coventry and Warwickshire) and the 2nd was with Dr Frederic Laude at Clinique du Sport in Paris, France.
No. It is fairly popular for surgeons to undertake sub-specialist fellowships but this is not a requirement. Some surgeons will enter practice straight from graduating the orthopaedic training program. Many surgeons who do undertake fellowships will do so locally in their home state or may travel interstate in Australia. Fellowships are often very poorly paid and so many doctors, with considerable debts from medical school and surgery training will not have the means to travel overseas for fellowship training. Mr Freedman was very fortunate to receive two scholarships (1. Arthritis Australia and 2. European Federation of Orthopaedics and Trauma) which enabled him to travel overseas twice for his international fellowship training.
Our locations
- Main Practice Consulting Rooms
- Other Clinic Consultations
- Surgery Operating locations
- Telehealth Consultations
Our main practice consulting rooms are located at:
Mr Ilan Freedman
Suite 2, Monash House Private Hospital
271 Clayton Road, Clayton VIC 3168.
Driving: Monash House Private Hospital is situated on Clayton Rd, across the road from Monash Medical Clinic. Clayton Road is easily accessible form Princes Highway (Dandenong Rd, North Rd or Centre Rd).
Parking: Parking available onsite (paid – inexpensive) and neighbouring streets (free)
Public transport: 3 minutes walk from Clayton Railway Station. Bus stop directly outside.
Location in the hospital: We are located on the ground floor, opposite the hospital coffee shop and next door to Capital Radiology
Mr Freedman also consults regularly at the following clinics.
Mulgrave Private Hospital Consulting Suites
Address: Blanton Dr, Mulgrave VIC 3170
Parking: Inexpensive onsite parking
The Bays Private Hospital Consulting Suites – Mornington
Address: Vale St, Mornington, 3931
Parking: Free Parking Available on site
Location: We are located in Suite 15 at The Bays.
Warragul
Address: 33 Victoria Street, Warragul 3820
Parking: Free Street Parking
Maryvale Private Hospital
Address: 286 Maryvale Rd, Morwell, 3840
Parking: Free Street Parking
Bay Street Specialist Centre
Address: Suite 4, 214 Bay Street, Brighton VIC 3186
Parking: Free Street Parking
Mr Freedman’s surgery operating locations are:
Mulgrave Private Hospital
Address: Cnr Police Rd & Gladstone Rd, Mulgrave, 3170
The Bays Private Hospital, Mornington
Address: 262 Main St, Mornington VIC 3931
Monash House Private Hospital
Address: 271 Clayton Rd, Clayton VIC 3168
Maryvale Private Hospital
Address: 286 Maryvale Rd, Morwell VIC 3840
Telehealth Consultation
We are pleased to offer telehealth appointments, allowing you to consult with Mr Freedman from the comfort of your home. Whether for a follow-up, pre-surgical consultation, or orthopaedic advice, our telehealth services provide expert care without the need to travel. Using secure and easy-to-use technology, our telehealth appointments fit seamlessly into your schedule, ensuring the same high standard of care as an in-person visit.

Get back to life sooner
We understand that seeking care for your hip or knee condition is an important decision, and we are here to provide you with the support and expertise you need.
Please take a moment to fill out the following information so that we can better understand your needs and how we can assist you.