Custom-Made Knee Replacement
Individualised implants for optimal outcomes
The future of knee replacement, today
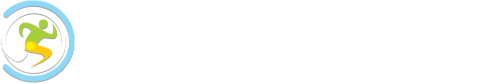
Custom Made Knee Replacement procedures represent a significant advancement in orthopaedic surgery, employing Patient-Specific Instrumentation (PSI) and cutting-edge 3D printing technology to produce customised implants for patients.
The procedure begins with a comprehensive 3D CT scan of the patient’s knee, which is processed by a team of biomedical engineers in Switzerland. A virtual 3D model of the knee is used to determine optimal implant size, shape and positioning. A 3Dprinted knee implant is then produced using high-grade materials to ensure durability and a precise fit.
The precision of this technology improves the accuracy of implant positioning. By ensuring an exact fit, these custom solutions assist rapid recovery and help to optimise patient outcomes.
The benefits of custom-made knee replacements
The advanced technology and procedures used in our custom knee replacement procedures have a range of benefits:
- Perfect Fit, Optimal Function: Custom knee replacement procedures use advanced 3D imaging and printing to create implants that match the unique contours of each patient’s knee, ensuring a perfect fit for optimum functionality and comfort.
- Reduced Surgical Risks: Using patient-specific data and implants these procedures may be less invasive, leading to reduced risk of complications, less postoperative pain, and quicker recovery times.
- Long-Lasting Implants: Our custom-made implants are crafted from high-grade materials using precise 3D printing techniques, resulting in a more durable and wear-resistant knee replacement that can withstand the demands of daily activity.

Case Examples
Robotic Knee Replacement
Robotic knee replacement surgery offers enhanced precision, customisation, and improved outcomes for patients. This procedure utilises robotic arms and computer technology to assist surgeons, enabling real-time imaging, precise bone cutting, and optimal implant placement based on the patient’s unique anatomy.
Mr Freedman starts with a CT scan to create a 3D model of the knee, helping with a detailed surgical planning. During the surgery Mr Freedman controls the robotic arm to execute the plan accurately, preserving healthy tissues.
The benefits include:
- Enhanced Precision: High accuracy in bone cutting and implant positioning, reducing the risk of misalignment.
- Customisation: Tailored surgery for each patient, ensuring a better fit and more natural function.
- Quicker Recovery: Less tissue damage leads to reduced pain, faster recovery, and a quicker return to daily activities.
- Extended Implant Lifespan: Accurate placement reduces wear and tear, potentially extending the implant’s lifespan.
- Better Outcomes: Improved range of motion and stability, enhancing the quality of life post-surgery.

Mr Freedman’s training & experience

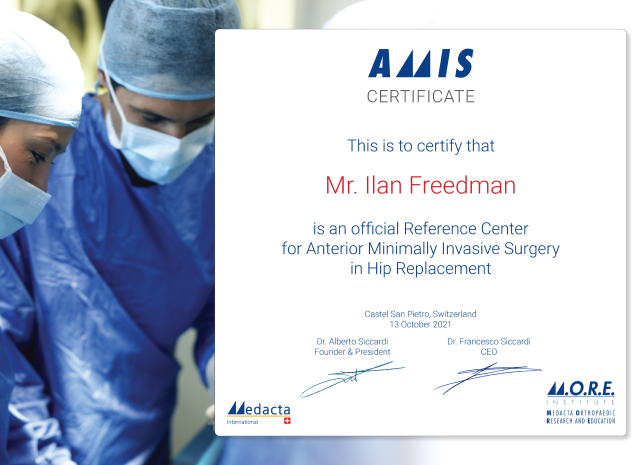
An Internationally-trained and renowned Orthopaedic surgeon, Mr Freeman brings over a decade of experience to providing a meticulous standard of care.
The success of technically complicated surgery depends on several elements, but one important factor is having a highly-trained and experienced surgeon.
Mr Freedman completed a fellowship in the UK to train in hip arthroscopy with Professor Damian Griffin, a world-renowned expert in hip arthroscopy and hip preservation surgery.
While on fellowship in the UK, Mr Freedman’s supervisor, Professor Griffin, received an invitation to observe a new hip replacement technique in Paris with Dr. Frederic Laude, a world expert in Direct Anterior hip surgery. As fate would have it, other commitments prevented Prof. Griffin from attending, so he sent Mr Freedman in his place, and he was amazed by the innovative procedure, the minimal incision, and the quick recovery of patients. Mr Freedman later returned to Paris to complete a fellowship under Dr Frederic Laude.
Upon returning to Australia, Mr Freedman, successfully implemented anterior approach hip replacements in his practice, leading to rapid growth in his case numbers and the eventual standardisation of this technique, even for complex surgeries.
-
Internationally Trained and Recognised
Mr Freedman has trained under some of the best hip surgeons in Europe.
-
Cutting-Edge Techniques
Mr Freedman employs advanced technology and techniques to ensure the best possible outcomes for his patients.
Precision-engineered implants
Our procedure uses advanced technology to create an implant designed specifically for your knee, ensuring perfect fit and optimised function.

Frequently asked questions
The implants that Mr Freedman chooses to use for most of his knee replacement procedures are Swiss made. The 3D-printed patient-specific instruments are also made in Switzerland.
No, not in Australia.
Personalised technology itself is expensive overseas as a high definition scan is performed, sent to expert engineers overseas who need to spend considerable time analysing the images, single use instruments need to be be made via 3D printing, sterilised and then couriered back to Australia but all this is FREE for Australian patients.
In Australia, the implant manufacturer is able to include this technology without additional cost to the patient.
No. PSI and robotics are both new technologies in knee replacement but work in different ways. In robotic knee replacement an intraoperative robot is used in the surgery to assist with implant positioning. In PSI knee replacement the surgery has been pre-planned with virtual simulation and then executed with 3D printed custom instruments.
A minor inconvenience is that it does take approximately 3-4 weeks for the patient-specific instruments to be manufactured in Switzerland and then delivered to Australia. Patients therefore need to wait a few weeks from their consultation until surgery.
This is usually not much of an issue as patients usually need some time to get themselves ready for surgery anyway, but this technology is therefore generally not used for urgent cases such as fracture care. If you require surgery urgently, Mr Freedman will perform your surgery through a more traditional (but still very reliable) technique.
Our locations
- Main Practice Consulting Rooms
- Other Clinic Consultations
- Surgery Operating locations
- Telehealth Consultations
Our main practice consulting rooms are located at:
Mr Ilan Freedman
Suite 2, Monash House Private Hospital
271 Clayton Road, Clayton VIC 3168.
Driving: Monash House Private Hospital is situated on Clayton Rd, across the road from Monash Medical Clinic. Clayton Road is easily accessible form Princes Highway (Dandenong Rd, North Rd or Centre Rd).
Parking: Parking available onsite (paid – inexpensive) and neighbouring streets (free)
Public transport: 3 minutes walk from Clayton Railway Station. Bus stop directly outside.
Location in the hospital: We are located on the ground floor, opposite the hospital coffee shop and next door to Capital Radiology
Mr Freedman also consults regularly at the following clinics.
Mulgrave Private Hospital Consulting Suites
Address: Blanton Dr, Mulgrave VIC 3170
Parking: Inexpensive onsite parking
The Bays Private Hospital Consulting Suites – Mornington
Address: Vale St, Mornington, 3931
Parking: Free Parking Available on site
Location: We are located in Suite 15 at The Bays.
Warragul
Address: 33 Victoria Street, Warragul 3820
Parking: Free Street Parking
Maryvale Private Hospital
Address: 286 Maryvale Rd, Morwell, 3840
Parking: Free Street Parking
Bay Street Specialist Centre
Address: Suite 4, 214 Bay Street, Brighton VIC 3186
Parking: Free Street Parking
Mr Freedman’s surgery operating locations are:
Mulgrave Private Hospital
Address: Cnr Police Rd & Gladstone Rd, Mulgrave, 3170
The Bays Private Hospital, Mornington
Address: 262 Main St, Mornington VIC 3931
Monash House Private Hospital
Address: 271 Clayton Rd, Clayton VIC 3168
Maryvale Private Hospital
Address: 286 Maryvale Rd, Morwell VIC 3840
Telehealth Consultation
We are pleased to offer telehealth appointments, allowing you to consult with Mr Freedman from the comfort of your home. Whether for a follow-up, pre-surgical consultation, or orthopaedic advice, our telehealth services provide expert care without the need to travel. Using secure and easy-to-use technology, our telehealth appointments fit seamlessly into your schedule, ensuring the same high standard of care as an in-person visit.

Get back to life sooner
We understand that seeking care for your hip or knee condition is an important decision, and we are here to provide you with the support and expertise you need.
Please take a moment to fill out the following information so that we can better understand your needs and how we can assist you.